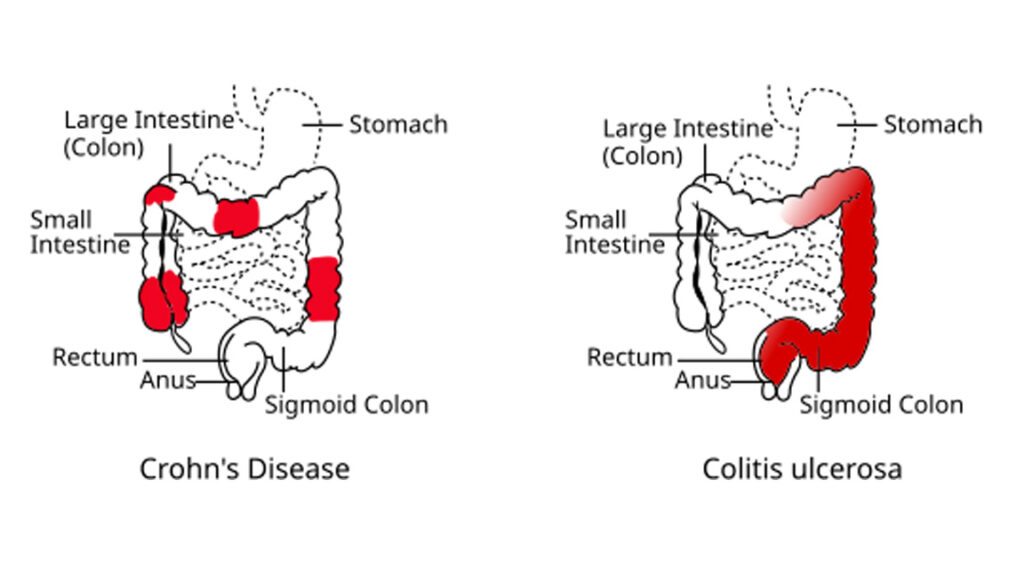
Crohn’s disease is not just a stomach problem. It’s a complex, chronic inflammatory condition that can affect any part of your gastrointestinal (GI) tract — from your mouth to your anus. While it often targets the small intestine and colon, its impact can ripple far beyond digestion, influencing your immune system, nutrition, and quality of life.
Globally, Crohn’s disease is on the rise. More than 10 million people worldwide live with this invisible burden — often diagnosed in their teens or early adulthood. It belongs to a broader category known as inflammatory bowel disease (IBD), but unlike other types, Crohn’s can burrow deep into intestinal walls and strike in unpredictable patches, making it notoriously hard to treat or manage.
What makes Crohn’s disease even more challenging is its uncertain origin. It doesn’t spread from person to person, and yet, no one fully knows what causes it. Genetics, immune dysfunction, environment, even your gut bacteria — all seem to play a part, but the exact recipe remains unsolved.
This guide dives deep into everything you need to know — from early warning signs and how it’s diagnosed, to medical treatments, dietary tips, daily challenges, and hopeful advances in research. Whether you’re newly diagnosed, supporting a loved one, or simply curious — this article will help you understand the full picture of Crohn’s disease in a clear, human way.
Symptoms & Early Signs of Crohn’s Disease
Crohn’s disease doesn’t knock on the door loudly at first. It often begins as mild discomfort, dismissed as stress, bad food, or a “sensitive stomach.” But beneath the surface, inflammation is quietly damaging the intestines — and over time, the signs become harder to ignore.
Here are the most common early symptoms that often appear during flare-ups:
1. Persistent Diarrhea
Unlike occasional loose stools, Crohn’s-related diarrhea is chronic. It can last for weeks and isn’t always relieved by over-the-counter medicine. It happens because inflammation in the gut interferes with your body’s ability to absorb water and nutrients properly.
2. Abdominal Pain & Cramping
Pain is often felt in the lower right part of the abdomen, but it can vary. It may come in waves — sharp during flare-ups, dull during remission. This pain results from inflammation, blockages, or ulcers in the intestinal lining.
3. Fatigue That Doesn’t Go Away
Not just tiredness, but deep fatigue — even after rest. Chronic inflammation, anemia (from internal bleeding), and poor nutrient absorption all drain energy levels. This exhaustion can severely affect work, relationships, and mental health.
4. Unintended Weight Loss
When your body struggles to absorb nutrients and food passes too quickly through your system, weight begins to drop. Appetite may decrease as well due to nausea, discomfort, or a fear of triggering symptoms.
5. Fever & Low-Grade Inflammation
A low-grade fever can be a subtle sign that your body is battling hidden inflammation. While it may seem minor, in the context of Crohn’s disease, it’s a signal worth noticing — especially when combined with other GI symptoms.
6. Mouth Sores or Ulcers
Painful ulcers in the mouth may appear — similar to canker sores — due to systemic inflammation. These are often overlooked but can be one of the early clues, especially in young adults.
7. Rectal Bleeding or Bloody Stool
If inflammation causes ulcers in the intestines, it may lead to bleeding — often visible in the stool. This symptom should never be ignored and is a key indicator of intestinal damage.
8. Skin Rashes & Joint Pain
Crohn’s doesn’t always stay in the gut. Some people experience skin inflammation, red or tender bumps (especially on the legs), or even arthritis-like pain in their joints.
Bonus: Silent Symptoms That Are Easy to Miss
Some signs are subtle but crucial:
- Loss of appetite
- Delayed growth in children
- Menstrual irregularities
- Eye inflammation (redness or vision changes)
These may not seem connected to digestion, but they’re all part of Crohn’s systemic impact.
What Causes Crohn’s Disease? Unraveling the Mystery
Despite decades of research, Crohn’s disease still carries an air of mystery. There’s no single “cause” — instead, it’s the result of multiple factors combining like a silent storm inside the body.
Let’s break down the most widely accepted causes and risk factors that science has uncovered so far.
1. Genetics: When It Runs in the Family
Crohn’s often runs in families. If a close relative — parent, sibling, or grandparent — has the condition, your chances of developing it increase significantly.
- Around 15-20% of people with Crohn’s have a first-degree relative with the disease.
- Specific genetic mutations (like NOD2 gene variants) are associated with a higher risk.
But here’s the truth: genes alone aren’t enough. You can carry the mutation and never get Crohn’s — which means something else needs to “trigger” it.
2. An Overactive Immune System
Normally, your immune system protects you from harmful bacteria and viruses. But in Crohn’s, something goes wrong.
- The immune system mistakenly attacks healthy gut cells, causing inflammation, ulcers, and long-term damage.
- Researchers believe the body may be reacting too strongly to normal gut bacteria or to a past infection that triggered an abnormal response.
Think of it as friendly fire — the immune system fighting a war inside your intestines, even when there’s no enemy.
3. Environmental Triggers: What You Breathe, Eat, and Live Around
Your surroundings may also play a role — especially in developed countries.
- Urban lifestyle, pollution, and processed food diets seem linked to higher Crohn’s rates.
- People in Western countries are more likely to develop it than those in rural or developing areas.
One theory is the “hygiene hypothesis” — in cleaner environments, immune systems may not get enough early exposure to microbes, leading to overreactions later.
4. Smoking: A Direct Risk Amplifier
Cigarette smoking is one of the strongest preventable risk factors for Crohn’s disease.
- Smokers are twice as likely to develop Crohn’s.
- It worsens flare-ups, increases complications, and slows healing after surgery.
This isn’t just correlation — nicotine and toxins directly damage intestinal tissue and increase inflammation.
5. Gut Microbiome Imbalance (Dysbiosis)
A healthy gut is home to trillions of microbes. But in Crohn’s patients, this balance often breaks down.
- “Good bacteria” levels drop.
- “Bad bacteria” or inflammatory strains may increase.
Whether this imbalance causes Crohn’s or results from it is still debated — but the link is undeniable.
6. Stress Doesn’t Cause Crohn’s — But It Makes It Worse
Let’s be clear: stress doesn’t cause Crohn’s. But it can trigger flare-ups, worsen symptoms, and affect recovery.
- Chronic stress affects gut motility, inflammation, and immune function.
- Mental health struggles like anxiety or depression are common among Crohn’s patients.
Managing stress is now a key part of long-term treatment — not just emotionally, but physiologically.
Bonus: Risk Factors You Can’t Control
- Age: Most people are diagnosed between 15–35 years old.
- Ethnicity: People of Ashkenazi Jewish descent have higher risk.
- NSAID Use: Regular use of ibuprofen or aspirin may irritate the gut and worsen symptoms.
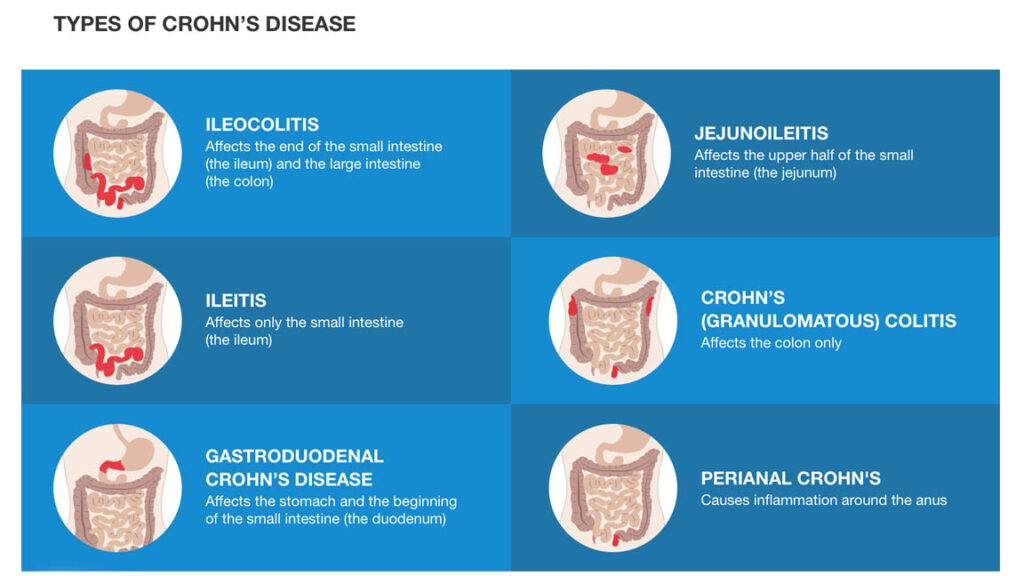
Image Credit: Blausen Medical Communications via Flickr, licensed under CC BY 3.0
Early Signs & Symptoms of Crohn’s Disease
Crohn’s disease doesn’t always start with intense pain or dramatic symptoms. In fact, the early signs are often mild, vague, and easy to ignore — which is why many people live for months (even years) without knowing what’s really happening inside their gut.
Here are some of the earliest signs that may indicate the onset of Crohn’s disease:
1. Persistent Diarrhea That Doesn’t Go Away
A major early symptom is frequent, watery diarrhea that lasts for weeks — even when there’s no food poisoning or stomach bug. This happens because Crohn’s disease causes chronic inflammation in the intestines, which interferes with normal absorption of fluids.
It’s not just occasional loose motion.
It’s daily disruption, sometimes 4–10 times a day.
And sometimes, it’s accompanied by an urgent need to run to the bathroom.
2. Abdominal Pain and Cramps (Usually Lower Right Side)
Early Crohn’s symptoms often include mild to moderate abdominal discomfort, especially after meals. The pain usually starts in the lower right quadrant of the stomach — but it can appear anywhere along the digestive tract, depending on which area is inflamed.
At first, it may feel like gas or indigestion.
But over time, the pain becomes sharper, more frequent, and harder to ignore.
3. Unexplained Fatigue and Low Energy
One of the most overlooked symptoms of Crohn’s disease is extreme tiredness, even after proper sleep. This fatigue comes from a combination of factors:
- Internal inflammation draining energy
- Poor nutrient absorption (especially iron)
- Disrupted sleep due to nighttime bowel issues
If someone feels “tired all the time” without reason — it’s not just lifestyle.
It could be Crohn’s beginning to show up in the background.
4. Weight Loss Without Trying
Crohn’s disease can reduce your appetite and make digestion less effective. People often start losing weight unintentionally — even though they haven’t changed their diet.
This can be an early sign that the body isn’t getting or absorbing what it needs.
It may also be tied to subconscious food avoidance, due to post-meal pain or diarrhea.
5. Mild Fever, Sometimes On and Off
In the early stages, a low-grade fever (around 99–100°F) may come and go. It’s often dismissed as a passing infection — but if it’s recurring or paired with gut issues, it might be a subtle sign of underlying inflammation.
This fever is usually caused by the immune system’s response to intestinal damage.
6. Bloating, Gas, or Feeling Full Too Quickly
People with early Crohn’s often complain about:
- Bloating
- Frequent belching or gas
- Feeling “heavy” even after small meals
This isn’t just discomfort — it’s because inflammation narrows the digestive passage, slowing down the food’s journey.
7. Mouth Sores (Aphthous Ulcers)
Crohn’s doesn’t just affect the intestines. In many cases, people develop small painful ulcers in the mouth, especially during flares. These can look like common canker sores — but they occur more frequently and may take longer to heal.
If mouth ulcers occur alongside stomach issues, they’re worth paying attention to.
8. Early Joint Pain or Skin Irritation
In some people, Crohn’s disease starts with extra-intestinal signs, meaning problems outside the digestive system. This includes:
- Mild joint pain (usually knees or ankles)
- Redness or inflammation on skin
- Eye irritation (like uveitis)
These might appear before gut symptoms fully show up — especially in immune-sensitive individuals.
When to Take Action
The danger with early Crohn’s disease is that the symptoms can be subtle — and often confused with IBS, stress, diet issues, or temporary infections.
But if someone experiences 3 or more of the above signs consistently for 4+ weeks, it’s time to talk to a doctor.
👉 Early diagnosis is the best way to prevent long-term damage.
The later Crohn’s is caught, the harder it is to manage — because intestinal scarring or narrowing may already have begun.
How Crohn’s Is Diagnosed: Tests, Scans & Medical Criteria
Crohn’s disease is a complex condition, and diagnosing it isn’t always straightforward. There’s no single test that confirms Crohn’s. Instead, doctors rely on a combination of clinical history, lab work, imaging, endoscopy, and biopsy results to reach a diagnosis. Let’s explore the complete diagnostic process:
1. Clinical Evaluation 👨⚕️
The first step is often a detailed review of symptoms and medical history. Your doctor will ask about:
- How long symptoms like diarrhea, pain, or fatigue have been occurring.
- Whether you’ve had weight loss or bleeding.
- Any family history of Crohn’s or inflammatory bowel disease (IBD).
This helps narrow down the possibilities and determine if Crohn’s is likely.
2. Blood Tests 💉
Blood tests are useful for identifying inflammation and nutritional deficiencies. They don’t confirm Crohn’s but provide important clues.
Common blood markers include:
- C-reactive protein (CRP): Elevated levels indicate inflammation.
- Erythrocyte Sedimentation Rate (ESR): Another inflammation marker.
- Complete Blood Count (CBC): Checks for anemia or infection.
- Vitamin B12 and Iron levels: To evaluate malabsorption.
3. Stool Tests 💩
Doctors may request stool tests to rule out bacterial, viral, or parasitic infections. These tests can also detect calprotectin and lactoferrin, proteins that signal intestinal inflammation — often elevated in Crohn’s.
4. Imaging Scans 🖼️
Imaging plays a critical role in detecting deep inflammation or damage to the intestines. Common scans include:
- CT (Computed Tomography) Scan: Offers a cross-sectional view of the intestines and can reveal thickened bowel walls or abscesses.
- MRI (Magnetic Resonance Imaging): Particularly useful for evaluating fistulas or perianal Crohn’s. MR enterography gives detailed images of the small bowel.
- Ultrasound: In some cases, especially in Europe, intestinal ultrasound helps detect bowel wall thickening or fluid buildup.
5. Endoscopy & Colonoscopy 📹
These are direct visual tools used to inspect the lining of your digestive tract.
- Colonoscopy: The gold standard for diagnosing Crohn’s. It allows doctors to see ulcers, strictures, or inflammation, and take biopsies from the colon and terminal ileum.
- Upper Endoscopy (EGD): If upper GI symptoms are present, this helps examine the esophagus, stomach, and duodenum.
- Capsule Endoscopy: Swallowing a camera pill can help visualize the small intestine — useful if traditional scopes miss abnormalities.
6. Biopsy and Histopathology 🧬
During endoscopy, small tissue samples (biopsies) are taken from the gut lining. These are examined under a microscope to:
- Look for granulomas (clusters of immune cells), which are often found in Crohn’s.
- Rule out other diseases like tuberculosis or ulcerative colitis.
7. Diagnostic Criteria and Differentiation 📋
Doctors combine all findings to confirm the diagnosis. They must also distinguish Crohn’s from similar conditions like:
- Ulcerative colitis
- Irritable Bowel Syndrome (IBS)
- Celiac disease
- Gastrointestinal infections
If inflammation appears in patches (“skip lesions”), affects any part of the GI tract, and reaches deep into the intestinal wall, it typically supports a diagnosis of Crohn’s disease.
Crohn’s Disease Treatment: Medical, Lifestyle & Surgical Options
Crohn’s has no known cure yet — but you can manage it, control flare-ups, and live a full life. Treatment plans are highly personalized, based on where the disease is, how severe it is, and how your body responds to different approaches.
Let’s explore the three pillars of Crohn’s disease treatment:
1. Medications: Controlling Inflammation & Symptoms 💊
Medication is usually the first line of defense. The goal is to reduce inflammation, manage symptoms, and prevent flare-ups or complications.
💡 Common Drug Categories:
- Aminosalicylates (5-ASAs)
Example: Mesalamine
Mild anti-inflammatory drugs. More effective in ulcerative colitis but sometimes used in Crohn’s. - Corticosteroids
Example: Prednisone
Powerful anti-inflammatories used short-term during flares. Not for long-term use due to side effects (weight gain, mood swings, bone loss). - Immunomodulators
Examples: Azathioprine, Methotrexate
Help calm the overactive immune system but can take weeks to months to start working. - Biologics
Examples: Infliximab (Remicade), Adalimumab (Humira), Ustekinumab
Target specific molecules in your immune system. Often used in moderate to severe Crohn’s. These drugs have revolutionized treatment for many patients. - JAK Inhibitors & Small Molecule Therapies
Newer oral medications (like Tofacitinib) are under research or used in specific cases. - Antibiotics
May be prescribed short-term to treat abscesses, fistulas, or infections associated with Crohn’s.
2. Lifestyle & Diet: Daily Choices That Make a Big Difference 🥗🚶
Your lifestyle doesn’t cause Crohn’s — but it absolutely influences how well you live with it. Here’s what you can control:
✅ Diet Tips for Crohn’s Patients:
- Low-Fiber During Flares: Helps reduce bowel irritation.
- Avoid Trigger Foods: Common culprits: dairy, spicy food, fried items, caffeine, alcohol.
- Stay Hydrated: Especially if diarrhea is frequent.
- Small, Frequent Meals: Easier on the digestive system.
- Vitamin Supplements: Especially B12, D, Iron, Zinc — often lost due to malabsorption.
💡 Pro tip: Keep a food-symptom diary to learn what works for your body.
✅ Lifestyle Habits That Help:
- Quit Smoking: Smoking worsens Crohn’s and increases flare-ups.
- Manage Stress: Yoga, journaling, therapy — stress can worsen symptoms.
- Exercise Regularly: Even walking reduces inflammation and improves mood.
- Get Enough Sleep: Crucial for healing and immune balance.
3. Surgery: When It’s No Longer Optional 🔪
Surgery is not a cure — but it can dramatically improve quality of life if medications fail or complications arise.
🏥 Common Surgical Scenarios:
- Bowel Resection: Removing the diseased part of the intestine.
- Fistula or Abscess Drainage: Especially around the anal area.
- Strictureplasty: Widening narrowed parts of the bowel without removing them.
- Ileostomy or Colostomy: In severe cases, part of the bowel is diverted outside the body.
📌 Fact: About 70% of Crohn’s patients eventually need surgery at some point — but many go years without needing it thanks to early intervention and biologic therapies.
Frequently Asked Questions (FAQ) on Crohn’s Disease
1. What is Crohn’s disease in simple terms?
Crohn’s disease is a chronic inflammatory bowel disease (IBD) that causes swelling and damage in the digestive tract—most commonly in the small intestine and colon. It can lead to symptoms like stomach pain, diarrhea, weight loss, and fatigue. It’s a lifelong condition that can come and go in flares.
2. How is Crohn’s disease different from ulcerative colitis?
Both are types of IBD (Inflammatory Bowel Disease), but Crohn’s can affect any part of the digestive tract (mouth to anus), and the inflammation can go through multiple layers of the bowel. Ulcerative colitis, on the other hand, only affects the colon and rectum, and inflammation usually stays on the surface layer.
3. What causes Crohn’s disease?
The exact cause of Crohn’s disease is still unknown, but research suggests a combination of genetic, environmental, and immune system factors. It is not caused by food or stress alone, although both can trigger or worsen symptoms. Family history and smoking also increase the risk.
4. Can Crohn’s disease be cured?
Unfortunately, there is no known cure for Crohn’s disease at this time. However, many treatment options—including medications, lifestyle changes, and sometimes surgery—can help manage symptoms, reduce inflammation, and improve quality of life. Some people can stay in remission for years.
5. What are the early symptoms of Crohn’s disease?
Early signs may include:
- Chronic diarrhea
- Abdominal pain or cramping
- Weight loss
- Fatigue
- Blood in stool
These symptoms can be mild and mistaken for other problems. Early diagnosis and treatment are crucial.
6. What foods should be avoided with Crohn’s disease?
While no single diet works for everyone, many people with Crohn’s report flare-ups from:
- Spicy foods
- High-fiber vegetables (like broccoli or cabbage)
- Dairy (if lactose intolerant)
- Fried or greasy foods
- Caffeine and alcohol
Working with a dietitian is recommended for a personalized plan.
7. Is Crohn’s disease dangerous?
Yes, if left untreated, Crohn’s can lead to serious complications such as intestinal blockages, malnutrition, fistulas, and even colon cancer. However, with proper Crohn’s disease treatment, many people live long and fulfilling lives.
8. Can stress trigger Crohn’s disease flare-ups?
Yes. While stress doesn’t cause Crohn’s, it can worsen symptoms or trigger flare-ups. Managing stress through therapy, mindfulness, exercise, or support groups is important for ongoing care.
9. Is Crohn’s disease genetic?
Crohn’s disease often runs in families. About 15-20% of people with Crohn’s have a first-degree relative with IBD. While genes increase the risk, they don’t guarantee the disease will develop.
10. How is Crohn’s disease diagnosed?
Doctors typically use a combination of tests including:
- Blood and stool tests
- Colonoscopy
- Imaging scans like CT or MRI
- Biopsies
These help determine the extent and location of inflammation in the digestive tract.
11. Can children get Crohn’s disease?
Yes. Crohn’s can affect children and teens, sometimes as young as 10. Pediatric Crohn’s may cause growth delays, fatigue, and digestive symptoms. Early diagnosis and child-friendly treatment plans are crucial.
12. What is the latest in Crohn’s disease treatment?
Modern Crohn’s disease treatments include:
- Biologics (like adalimumab and infliximab)
- Immunomodulators
- Advanced oral therapies
- Nutritional therapy
- Surgery (in severe or unresponsive cases)
Ongoing research is exploring stem cell therapy and microbiome-targeting treatments.
Final Thought
Crohn’s Disease is not just a gastrointestinal condition — it’s a chronic, life-altering journey that affects how a person eats, lives, and even thinks about their future. While there’s still no known cure, today’s advancements in Crohn’s Disease treatment, from targeted biologics to personalized care plans, offer real hope.
What truly makes a difference, however, is awareness and early action. Listening to your body, recognizing symptoms early, and consulting the right specialists can drastically improve outcomes. Whether you’re newly diagnosed, living with it for years, or supporting a loved one — remember: You’re not alone.
At its core, managing Crohn’s is about building a lifestyle that supports healing — through informed choices, ongoing support, and medical guidance.
📲 Let’s Stay Connected
🔎 Want to explore more health guides like this?
Visit our full article collection here: Pneumonia: Causes, Types, Symptoms Why It Still Matters
👉 https://evichar.com/pneumonia-symptoms-causes-treatment-prevention-guide/
💬 Follow us for regular updates, health insights, and awareness posts:
👉 E-Vichar on Facebook
Image Credit: Wikimedia Commons, licensed under Creative Commons Attribution-ShareAlike 3.0 (CC BY-SA 3.0)